What is Urethral Cancer?
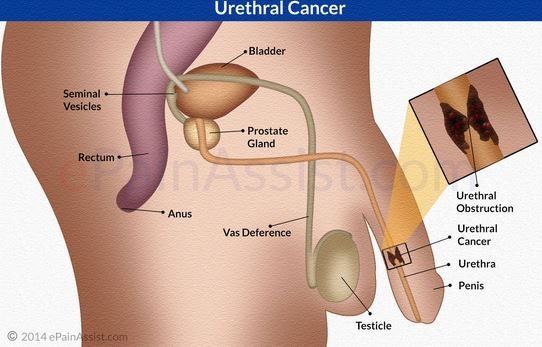
Urethral cancer (UC) is the rarest type of urological cancer, with less than 2000 known cases. Urethra is a tube-shaped organ that connects the bladder with the urethral opening for the removal of urine. Males and females have a different anatomy of the urethra, and it plays a role when deciding on treatment. UC is a carcinoma- it develops from cells of the urethral lining[1].
Causes
The exact causes of UC are not known. There are risk factors that have been associated with UC:
- Chronic irritation of urethra
- Infection- sexually transmitted diseases, HPV
- Arsenic ingestion has been linked to UC
- Exposure to radiation (for example-previous cancer treatment)[2]
Symptoms
Initially there might be no symptoms. Mostly the symptoms are associated with narrowing of the urethra, like trouble emptying the bladder or overflow incontinence. More specific symptoms are perineal pain and haematuria. Other symptoms include:
- Diminished stream of urine
- Voiding sensation
- Frequent urination, also during night
- Itching
- Purulent or watery, smelling discharge
- Pain in the pubic area
- Haematospermia
- Swelling of the urethral opening
- Pain during intercourse[2]
Diagnosis
Physical examination
During physical examination, some signs can be found that suggest UC:
- Fistula from urethra to the skin
- Regional lymph nodes enlarged and painful
- Bloody or mucosal discharge from urethra
- Fistula to the vagina
- Urethral diverticula
- Abscess or tissue necrosis
- Lesions of the penis or vagina
- Palpable mass [4,1]
Laboratory studies
There are no blood analyses that can prove the diagnosis of UC. Usually they are used for differentiating UC from an infection. Increased alkaline phosphatase levels can suggest skeletal metastases. Urine analysis and culture should be performed in order to exclude infection[4].
Histology
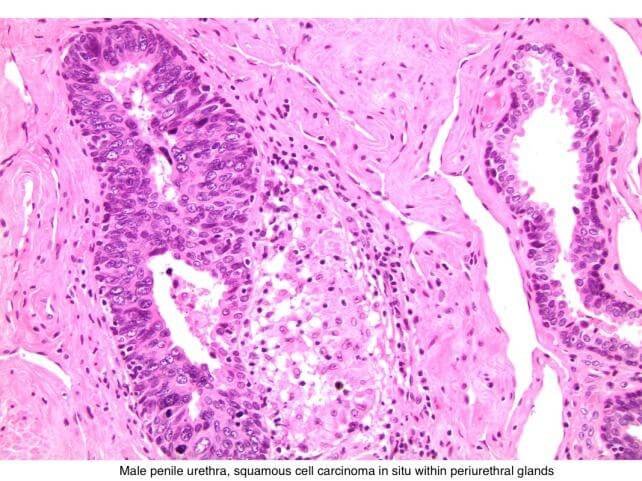
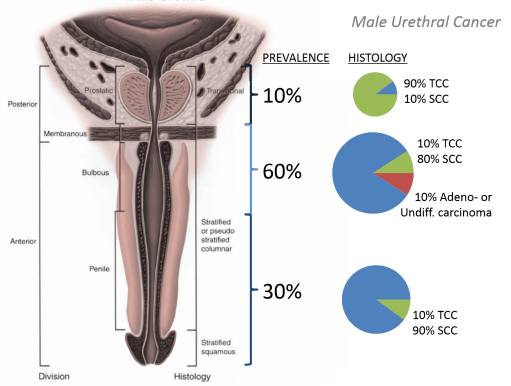
To confirm the diagnosis, usually transurethral biopsy is performed. During this procedure a sample of tissue is taken to further evaluate it[4]. There are 4 histological types of urethral cancer:
- Urothelial carcinoma- with malignant cells that resemble the epithelium of bladder (also see transitional cell carcinoma)
- Squamous cell carcinoma– composed of sheets of large tumor cells in various shapes
![]()
- Adenocarcinoma- composed of simple columnar epithelium (also see bile duct adenocarcinoma)
- Clear cell adenocarcinoma- cuboidal, different sized cells (also read about clear cell renal cancer) [7]
![]()
Imaging studies
MRI is the method of choice in diagnosing UC.MRI shows the extent of disease and can help in planning the treatment. MRI can also help the assessment of therapy.
CT and X-ray of the chest, pelvis and the abdomen is also helpful in assessing metastatic distribution of UC[4].
Other tests
Flexible cystoscopy is a minimally invasive procedure during which a flexible tube with camera is inserted into urethra to visually evaluate it. During cystoscopy a papillary mass, erythematous areas or ulceration of the mucosa can be seen, and it can suggest cancer [4].
Staging
Staging of any cancer is important part of planning the treatment. UC is staged based on the TNM classification- tumor, node, and metastasis.
T-primary tumor
- Tx- primary tumor cannot be assessed
- T0- no evidence of primary tumor
- Ta- non-invasive carcinoma
- Tis-carcinoma in situ
- T1- tumor invades subepithelial connective tissue
- T2-tumor invades corpus spongeosum, prostate (in men) or periurethral muscle (in women)
- T3-tumor invades corpus cavernosum, tissue beyond prostatic capsule (in men) or anterior vagina, neck of the bladder (in women)
- T4- tumor invades other organs- the bladder
N- lymph nodes
- Nx- lymph nodes cannot be assessed
- N0- no metastasis in regional lymph nodes
- N1- metastases in single lymph node, not bigger than 2cm
- N2- metastases in single lymph node, bigger than 2cm, but smaller than 5cml
- N3- metastases in lymph node that are larger than 5 cm
M-metastases
- Mx- metastases cannot be assessed
- M0- no metastases
- M1- distant metastases present (most commonly liver and lungs)[2]
Treatment
Therapy for urethral cancer varies with the stage and location of the tumor. Since this tumor is so rare, there is no statistically certain choice for treatment[4,5].
Radiation therapy
Radiation therapy is used as primary treatment option, as well as combination together with chemotherapy and/or surgery. In small, early stage lesions radiation can be very successful and the treatment will not require surgery. Radiation also has high rate of success in woman, because surgery has significantly higher risk of morbidity [4,5].
Chemotherapy
Chemotherapy is sometimes used alone, but more often together with radiation therapy. The data about the effects of chemotherapy are limited. Similarly to squamous cell cancer, chemotherapy regime of methotrexate, vinblastine doxorubicin and cisplatin is used in combination with radiation for locally advanced disease[4,5].
Surgical treatment
Surgery is the method of choice for both males and females. The extent of surgical treatment depends of the stage and location of the cancer. There have been 4 methods described for surgical treatment:
- Conservative therapy and local excision
- Transurethral excision of low grade tumor
- Endoscopic treatment with transurethral electro-resection or laser therapy
- Segmental resection with reconstruction- a part of urethra is removed, and the healthy part is mobilized to create new urethral opening. Not usable for woman.
- Partial penectomy
- Excision of the lesion with around 2cm margins
- Can be used for distal, infiltrative tumors in men
- Radical penectomy
- Removal of the penis, urethra and penile root
- En block resection
- For tumors higher than T2 stage in the prostatic part of urethra
- Procedure includes removal of the affected urethra as well as local lymphnodes
- In women portions of perineal tissue also are removed
- In women most cases require removal of the vagina [5]

 Prognosis
Prognosis
Urethral cancer is very rare and the treatment usually is very aggressive. Despite aggressive treatment with radiation, chemotherapy and surgery, recurrence rate is more than 50%. Due to the aggressive treatment, many patients experience complications:
- Stricture (narrowing) of urethra
- Inflammation of bladder and urethra caused by radiation
- Bowel irritation
- Fibrosis
- Bleeding
- Formation of fistula
- Secondary cancer[6]
Survival rate
Both sexes
- Age- more than 65 years and African American race
- Size, tumor location
- Stage, grade, involvement or lymph nodes and metastasis
- Type of treatment
- Presence of concomitant bladder cancer
For men:
- Invasion of the cancer in prostate
- Invasion in lymph vessels and nerves
- Tumors in the proximal urethra have a worse prognosis.
The 5 year survival rate depends on the stage of the tumor. For lower stage tumors it is around 83%, while in later stage tumors the survival rate is around 45% [6].
If you found this article helpful, share it on social media. For your personal experience and comments use the box below.
References
- General patient information: http://www.webmd.com/cancer/tc/urethral-cancer-treatment-patient-information-nci-pdq-general-information-about-urethral-cancer
- Causes and staging: http://www.urologyhealth.org/urologic-conditions/urethral-cancer/causes
- Symptoms: http://www.medicinenet.com/urethral_cancer/page2.htm
- Diagnosis: http://emedicine.medscape.com/article/451496-workup#c4
- Treatment: http://uroweb.org/wp-content/uploads/08-Primary-Urethral-Carcinoma_LR1.pdf
- Prognosis and relevant anatomy: https://www.cancer.gov/types/urethral/hp/urethral-treatment-pdq
- Histology and prognostic factors: http://www.pathologyoutlines.com/topic/urethracarcinoma.html
Similar Posts:
- Vaginal Cancer – Symptoms, Signs, Pictures, Treatment, Causes
- Vulvar Cancer
- Duodenal Cancer – Symptoms, Prognosis, Survival Rate and Treatment
- Lip Cancer
- Gum Cancer – Pictures, Symptoms, Signs, Treatment, Complications
- Appendix Cancer – Symptoms, Survival Rate, Prognosis, Treatment,
- Medullary Thyroid Cancer – Symptoms, Treatment, Prognosis






Leave a Reply