What is a Precancerous Mole?
Precancerous Mole is a pigment growth on the skin, more precisely a benign growth of melanocytes- cells that give the skin its color. Over time, abnormal moles can develop into melanoma- skin cancer.
It is important to recognize atypical moles and follow their development. Atypical moles belong to a group of precancerous skin conditions, that have the potential to cause cancer [1].
Risk factors
Ordinary moles rarely develop into cancer, but atypical moles are more likely to cause cancer. There is no certain timeline for when the mole could become cancerous- in some cases a person can live their whole life without developing skin cancer.
Main risk factor for developing skin cancer from precancerous mole is if the patent is suffering from Familial dysplastic multiple mole melanoma syndrome. FAMMM is an autosomal dominant condition, where a person has more than 50 moles on their body and a family history of melanoma (also read about Uveal melanoma).
It is associated with a certain gene mutation, but it has variable expression and penetrance, meaning that not all the family members who inherit the gene will develop melanoma. This syndrome is also associated with pancreatic cancer [2].

Another risk factor is atypical mole syndrome. Unlike FAMMM, his syndrome is not genetic.
It is characterized by having:
- 100 or more moles
- One or more moles are larger than 8mm in diameter
- One or more moles are atypical [4]
Signs
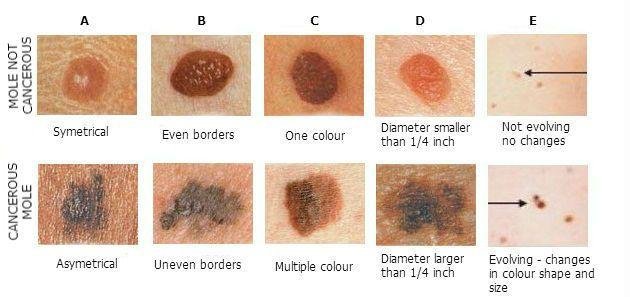
The signs and symptoms of a precancerous mole are:
- Diameter larger than 6mm
- Irregular shape
- Irregular, faded borders
- Centrally raised surface
- Rough surface
- Multiple colors- pink, red, brown [3].
![]()
Usually the symptoms of atypical.
- A- asymmetry of the mole
- B-borders, irregular, faded
- C-color, multiple colors
- D-diameter, larger than eraser on a pencil
- E-evolving- if the mole is growing or shrinking, starts to change color or bleed, it should be checked out [1].
Another type of precancerous moles are congenital melanocytic nevi- birthmarks that are present at birth or develop during early childhood. Symptoms of congenital melanocytic nevus are:
- Brown or black color
- Raised above the skin
- Coarse, dark hair on top
- Irregular surface
- Irregular or regular borders [3]
Diagnosis
Physical examination
If the patient has noticed a suspicious mole, it must be examined. Patients should follow changes in their moles and do self-check once in a while. Examination usually consists of the ABCDE’s as mentioned before. If you want to learn about other malignant skin conditions, read about Keratoachantoma and Squamous cell carcinoma.
Skin biopsy
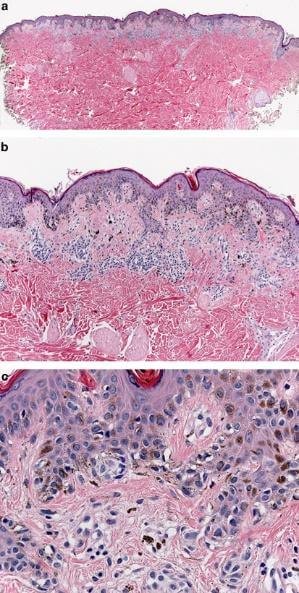
The most accurate way of telling if the mole is benign, precancerous or malignant, is to do a skin biopsy. Usually skin biopsy is done if the doctor suspects possible malignant changes. Biopsy material can be acquired by using punch biopsy or completely removing the mole. Atypical moles are characterized by two major categories of criteria- architectural and cytological:
- Larger than common nevus
- Contain a junctional component with normal skin
- Increased number of melanocytes, especially in the junction zone
- Dermal fibroplasia, associated with lymphocytic infiltrate
- Atypical cells with enlarged nucleus, irregular shape and hyperchomasia-clumps of chromatin [5]
![]()
Genetic changes
Recently, scientists at Johns Hopkins center have discovered a link between skin cancer and two genes, that can trigger the development of skin cancer. These genes can become an important marker for early diagnostics. In melanoma, the cell growth regulatory gene Id1 deactivates a tumor suppressor gene p16/Ink4a.
Tumor suppressor genes are usually active and prevent normal cells to develop into cancerous cells (also see Trichoepithelioma). High Id1 protein levels can be found in the first stages of melanoma therefore the condition can be diagnosed early. Still, more studies are needed to confirm this protein as a definite diagnostic marker [6].
Treatment
Usually precancerous moles do not require treatment. They should be observed by the patient and family doctor for suspicious changes. Best way to observe the moles in long term is to take photos of them for later comparison. In case the mole changes its appearance, or starts to bleed, removal should be considered.
Also, atypical moles are often surgically removed for cosmetic reasons, or because they get traumatized. Surgical excision in local anesthesia can be performed for smaller lesions. In some cases, general anesthesia is necessary. The mole should be removed with clear margins so that any possible malignant cells are not left in the skin.
Although laser removal is sometimes used, this method is not indicated, since it doesn’t penetrate deep tissue enough to remove all the lesion, and there is no tissue samples left afterwards for examination.
Complications after removal of the precancerous mole can be bleeding, scarring and infection, as well as reaction to the anesthetic. In case the mole quickly regrows, immediate medical attention should be sought [7].

![]()
If you found this article helpful, share it on social media. For your personal experience and other comments use the section below.
References:
- What is a precancerous mole: http://www.webmd.com/melanoma-skin-cancer/ss/slideshow-skin-lesions-and-cancer
- https://www.ncbi.nlm.nih.gov/books/NBK7030/
- http://www.cancer.ca/en/cancer-information/cancer-type/skin-melanoma/melanoma/precancerous-conditions/?region=on
- http://www.skincancer.org/skin-cancer-information/atypical-moles
- Histological changes: http://www.nature.com/modpathol/journal/v19/n2s/full/3800515a.html
- Genetics: http://unisci.com/stories/20013/0816013.htm
- Treatment: http://www.emedicinehealth.com/mole_removal/page3_em.htm#during_the_mole_removal_procedure
Similar Posts:
- Ocular Melanoma
- Amelanotic Melanoma – Pictures, Symptoms, Prognosis
- Uveal Melanoma
- Tumor Suppressor Genes
- Choroidal Melanoma
- Rhabdoid Tumor
- Choriocarcinoma – Symptoms, Prognosis, Treatment, Diagnosis






Leave a Reply