Definition
Cholangiocarcinoma abbreviated as CCC are malignant growths that arise within the biliary duct system, originating from either the internal side or the external side of the liver, from the extrahepatic bile ducts, and then terminating at the ampulla of Vater.
This health problem is the same as cancer of the bile duct. Above 90% of CCC cases are ductal adenocarcinomas and the rest are found to be squamous cell tumors. Its occurrence rate is 1-2 for every 100,ooo population each year; where males are more affected compared to females and manifested by individuals who are 60 years of age and above.
Symptoms of Cholangiocarcinoma
The characteristic clinical manifestations of cholangiocarcinoma include:
- Jaundice – This has been noted to be the most common symptom of cancer involving the bile duct, and this is easily best detected when the person is exposed under direct sunlight exposure. This is observable in the later part of the intrahepatic tumors or perihilar tumors and considered as a marker for a developing advanced disease condition.
- Weight loss – Decrease in weight can vary among patients.
- Abdominal pain – Abdominal pain pointed out as dull ache found in the right upper abdominal quadrant is relatively seen in advanced cases of CCC.
- Liver function tests which are not within the normal range
Some other symptoms of an affected person can be:
- Dark-colored urine changes
- Clay-colored stools
- Presence of fever
- Generalized itching of the body – Pruritus is mostly preceded by the person’s jaundice; however it can also be an initial sign of CCC. This is linked with the circulating bile acids in the biliary tree.
- Hepatomegaly may also develop
- Splenomegaly can be formed if there will be a prolonged biliary obstruction as a result of a secondary type of biliary cirrhosis
- Courvoisier’s sign or a palpable bladder can be felt when there are tumors that exist on a distal point to the cystic duct
Pathophysiology
Cholangiocarcinoma are malignant tumors which are slow-growing and it can locally spread to other areas through a lymphatic system route and involving local structures like some blood vessels that feed the liver. The exact etiologic factor is yet unknown.
Common sites affected by cholangiocarcinoma:
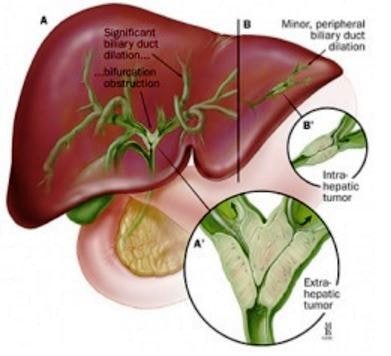
- CCC affects usually the perihilar region which is located near the branching out portion of the right hepatic duct and the left hepatic duct like in cases of the classical Klatskin’s tumor.
- The next type that commonly develops is the distal extrahepatic tumors which are located between the ampulla of Vater and the pancreatic upper border.
- The least that may come out is in the form of an intrahepatic tumor.
Predisposing risk factors which might lead to CCC development are:
- Patients having chronic ulcerative colitis
- Infection with liver flukes
- Industrial chemical exposure
- Thorium exposure
- Congenital problems of bile ducts
- Caroli’s disease
- Patients with HIV, hepatitis C, diabetes mellitus and liver cirrhosis
Diagnosis
Clinical diagnosis is being confirmed based on the results of the following examinations:
- Radiological investigations like the CT or MRI imaging
- Pathological assessment done from a tissue biopsy
- Fine needle aspiration procedure
- Biliary brush cytology test
Diagnostic test findings can be as follows:
- Liver function tests showing an elevated level of conjugated bilirubin
- Prolonged prothrombin time and international normalized ratio
- Tumor markers may appear raised
- Ultrasound and CT scan results showing dilated intrahepatic biliary tree
- Contrast MRI for optimal imaging of an existing CCC, but is way below to the efficiency of CT to detect metastasis to other areas of the body
- MRI (magnetic resonance imaging) cholangiography or ERCP (endoscopic retrograde cholangiopancreatography) showing evidence of an obstructed site in the biliary system
- Angiography is done prior to any surgical intervention linked with CCC to visualize arteries and veins
Different Staging of Cholangiocarcinoma
The staging process for cancer of the bile duct is a very significant factor needed to select treatment options available and to estimate for a patient’s prognosis in relation to CCC. Staging is being determined through the results of physical examination done, diagnostic tests and imaging tests done, and the outcome of any surgery when already performed to the patient.
The American Joint Committee on Cancer TNM system is the main system being used for the staging of cholangiocarcinoma. There are three various staging systems which are utilized among patients with cancer of the bile duct, and this depends on which specific location did it start to develop such as:
- Intrahepatic cancer of the bile duct that starts within the liver
- Perihilar cancer of the bile duct which starts at the hilum point, just on outside of the liver
- Distal cancer of the bile duct which starts on an area farther from the biliary duct system
There are 3 pieces of information provided by the TNM system for staging cancer of the bile duct and they are:
- T is used to describe if the primary tumor that arise has reached the bile duct wall and whether it has affected some other nearby body organs or tissues
- N is used to describe if the cancer has successfully spread itself to some nearby or regional lymph nodes
- M is used to describe if the cancer has been able to metastasize to nearby organs of the body, which might be the liver, the peritoneal cavity and the lungs
Treatment
Cholangiocarcinoma as a form of cancer is incurable and can be deadly, unless all the malignant tumors are surgically resected or totally removed.
Medical treatment of CCC involves any of the following:
- Stenting is used if the tumor is not possible for resection
- Photodynamic therapy (PDT) to restore biliary drainage and to improve the quality of life among patients
- Radiation therapy to reduce tumor size and make them possible for resection
- Chemotherapy as radiation sensitizer for patients
- Complete surgical resection of existing tumors is the lone therapy for cure
Survival rate
The survival rate is basically low since about 90% of cases are not possible to have the curative resection performed. The complete removal of the malignant tumor may reach the 5-year survival from 1 among 5 patients with greater chance of complete cure with CCC. Rates can vary as 0% for nonresectable cases, with less than 5% survival in general; and 10-40% 5 year survival rates for those with surgery.
Prognosis
Cure from CCC is not generally possible in the failure of tumor removal. For those who undergo treatment, half among them may live a year more, and about half of them may live longer, but very rare to live beyond 5 years.
Foundation
CCC foundation as a nonprofit organization aims at the cure for cancer of the bile duct through goals directed at collaboration, understanding, research and extension principles. They provide support to patients, advocate for them and make them understand more about CCC.
References
- http://emedicine.medscape.com/article/277393-overview
- Cholangiocarcinoma – Epidemiology, Presentation, Investigations, Differential diagnosis, Staging, Management, Complications, Prognosis at http://patient.info/doctor/cholangiocarcinoma
- http://www.cancer.org/cancer/bileductcancer/detailedguide/bile-duct-cancer-staging
- https://www.linkedin.com/company/the-cholangiocarcinoma-foundation
- Singal AK, Vauthey JN, Grady JJ, Stroehlein JR (2011 Jul). Intrahepatic cholangiocarcinoma–frequency and demographic patterns: thirty-year data from the M.D. Anderson Cancer Center. J Cancer Res Clin Oncol. 137(7):1071-8.
- Uchida M, Ishibashi M, Tomita N, et al (2005 May). Hilar and suprapancreatic cholangiocarcinoma: value of 3D angiography and multiphase fusion images using MDCT. AJR Am J Roentgenol. 184(5):1572-7.
- Clary B, Jarnigan W, Pitt H, et al (2004 Mar-Apr). Hilar cholangiocarcinoma. J Gastrointest Surg. 8(3):298-302.
Similar Posts:
- Klatskin Tumor
- Stage 4 Liver Cancer (End Stage) – Life Expectancy, Survival Rate
- Duodenal Cancer – Symptoms, Prognosis, Survival Rate and Treatment
- DCIS Breast Cancer
- Urethral Cancer
- Krukenberg Tumor
- Malignant Mesothelioma






Leave a Reply