Anaplastic Astrocytoma is a type of cancer that often affects the brain. The word anaplastic or anaplasia denotes the backward differentiation of cells linked to malignancy. It may also refer to the increased ability of cells to multiply. Such a lack of differentiation and upsurge in reproduction are the trademarks of aggressive malignancies. Astrocytes on the other hand refer to the supportive tissues of the brain. These cells are highly distinguishable from other cells because of their highly defined star-form. Therefore, anaplastic astrocytes refer to the cancer of the astrocytes found in the brain.
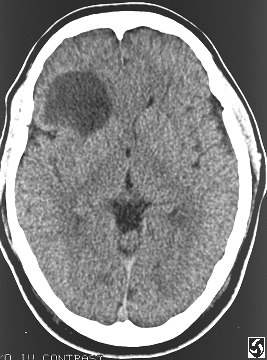
Anaplastic Astrocytoma as seen in an MRI
Symptoms
Since this condition is found in the brain, most of its symptoms are neurological in nature, most of which stem from increased intracranial pressure. The common symptoms include:
- Headache
- Vertigo
- Nausea and Vomiting
- General Body Malaise
- Motor Deficiencies
- Hormonal Imbalances
- Change in Consciousness, Thought Process, Behaviour and Orientation Problems
- Seizures
Causes
Most cases of anaplastic astrocytoma do not have definite causes, meaning the disease happens sporadically and there is not much that can be done to prevent it. Studies however reveal that it has close links to families that have:
- Neurofibromatosis Type I
- Li-Fraumeni Syndrome
- Heritable Non-polyposis Colon Cancer
- Tuberous Sclerosis
Other causes:
- Exposure to vinyl chloride
- High doses of radiation.
Classifications
The World Health Organization identified four grades for classifying Anaplastic Astrocytoma depending on the cell’s speed to multiply and spread to surrounding tissues. Noninfiltrating astrocytomas grow at a slower pace than infiltrating ones and are less common than the infiltrating types or diffuse astrocytoma.
Grade I
This grade is often the noninfiltrating type. One of its kind is the ACOUSTIC NEUROMA which affects the eight cranial nerves affecting one’s hearing and balance. It may grow at a sluggish pace but can grow to a really big size. Children and teens are often the ones affected by this grade.
Grade II
This grade covers infiltrating tumor also called as low-grade astrocytoma. The features of its tumor include growing really slow without well-defined borders. This is most prevalent among adults between the age ranges 20-40.
Grade III
It is also called as anaplastic or malignant astrocytoma because compared to the other grades it grows rather quickly and is common among adults aged 30 to 50. It accounts for 4% of all brain tumors. 30-40% of patients are able to survive for 3-5 years.
Grade IV
It is more commonly called Glioblastoma (GBM)which is the most aggressive kind of brain tumor. It is also known as Glioblastoma Multiforme because of the many structures it can take when viewed under the microscope. It affects mostly older individuals aged 50-80 and it accounts for 23% of all primary brain tumors. Patients have decreased chances of surviving this type compared to those in Grade III as they are only given 2 years to survive.
Treatment
It will be the physician’s role to suggest the right and specific intervention needed to address the specific type of brain tumor. The physician’s choice will depend on the client’s age, overall health and health history, characteristics of the tumor (type, location, size), extent of the illness, ability to withstand specific medications, procedures or therapies, and the doctor’s perception on the progress of the disease. The patient’s opinion or preference may also be taken into account.
The following treatment interventions may be used alone or in combination:
- Surgery. This may be done for a number of reasons such as treatment of increased intracranial pressure, biopsy and removal of the tumor. Other than that, it can be practiced to facilitate rightful assessment of the disease condition through modern technology such as intra-operative MRI.
- Radiation Therapy. This is the use of strong-energy radiation rays to shrink and eventually kill tumor cells. Precautionary measures should be practiced in order to avoid the unnecessary complications of radiation therapy.
- Chemotherapy. This occurs with the use of pharmacological therapies to stop the progress of cancer cells. It aims to attack and avoid the spread of the cancerous cells. For it to be a lot more effective, it can be used in combination with other chemotherapy agents.
Prognosis
Prognosis is done on the patient’s brain tumor so that scientists and other health professionals can come up with a possible cure or treatment to control the illness. It will help patients live a little longer and happier. It shows that the adverse effects experienced will only worsen if no immediate and appropriate medical attention is provided for the patient.
Survival Rate
This condition’s prognosis has come to 3 major conclusions about the patient’s survival rate through its retrospective studies.
- There is a high probability of 83% chance of surviving or 10 years of overall survival if diagnosed early on and proper interventions are made. If the tumor hasn’t been completely removed, half of the patients are expected to live for the next 5 years.
- For those with cases of juvenile pilocytic, prognosis reveals that the patients who have been asymptomatic for 5 years have a 60% chance of surviving and a 85% chance for those with 10 years of being symptom-free. The strongest predictor of the outcomes is the extent of the surgical resection. Those with total resection have the highest survival rate.
- Anaplastic astrocytoma prognoses with High Grade Astrocytoma among youngsters are poorly appreciated. They have a survival rate of 15-20 % when different treatment approaches have been practiced in combination with others such as chemotherapy and radiotherapy. Outcomes may increase if a full tumor resection has been sought.
Life Expectancy
Generally, a patient is given five years to live if all treatments have been exhausted without success. The reason behind this is the fact that total removal of the tumor is generally impossible, thus increasing the chances of relapse. The life expectancy depends on the amount of tumor removed and how it has already affected the overall brain function of the patient.
Further Reading:
http://csn.cancer.org/node/162906
http://nyp.org/health/anaplastic-astrocytomas.html
http://brain.mgh.harvard.edu/glioblastoma.htm
Similar Posts:
- Anaplastic Thyroid Cancer – Symptoms, Treatment, Prognosis
- Glioblastoma Multiforme – Life Expectancy, Stage 4, Survival Rate, Symptoms, Prognosis
- Inoperable Brain Tumor
- Urothelial Carcinoma
- Ganglioglioma
- Wilm’s Tumor
- Leiomyosarcoma – Survival Rate, Symptoms, Prognosis, Treatment






my husband was recently diagnosed with anaplastic astrocytoma between stage 2 and 3.
What is the prognosis with radiation and chemotherapy. Everything I have read points to about 5 years. I want to know what the basic prognoses is. Is there anyone who can at least try and tell me.
🙂
i have Anaplastic.Astrocytoma. Stage 3. They Didnt Get It All Out. But I Have Not Done Any Chemo/Radiation. I Have Lived For 15 Years Now. But I An Starting To Get Those Bad Server Headaches Again. Im Getting Dizze Again An My Balance Is Off Again Going To Get A Check Up On My Head Next Month . Thats The Soonest They Can See Me. Thats My Email At The Top.
I was diagnosed in 2003 and had surgery that removed 90% of the tumor. I then went through chemotherapy (temodar) and radiation. So far I haven’t had any recurrence or re-growth of the tumor. Ten years on Nov. 25th.
Matt would you mind telling what stage your tumor was and what symptoms you experienced? I am so very happy to hear of your success and wish you continued health. Thank you,
Kathy
I had a grade 3 anaplastic astrocytoma and I had very few symptoms. I remember having a loss of where I was. I mean I knew where I was but it was like every hallway was new and not there before. I had one seizure which was what caused me to go to the hospital and was later diagnosed with the tumor. 90% was removed and I was later treated with Temodar and radiation.
I’m so sorry to hear about your husband. I have been diagnosed with grade III anaplastic astrocytoma and everything the doctors have said about prognosis is directly related to how much residual tumor is left over after resection/surgical intervention. Highest life expectancy/survival with total resection of tumor. Did your husband have surgery or is that even a possibility depending on location of tumor?
Thinking of you and your family. If I can help in any way let me know.
Heidi
My sister-in-law was just diagnosed yesterday with Anaplastic Astrocytom G3. Just trying to figure out where to start to find a specialist that would consider surgery. I hope you are doing well.
Dr.Carlo Pulaseo in Portsmouth N H.He is awesome and saved my sons life.
This past summer my son-in-law was diagnosed with Anaplastic Astrocytoma G3. He went to Dr. Anton of the Cleveland Clinic who performed the surgery to remove the tumor.
Dr. Anton was the second opinion. The first thought it was benign and didn’t want to do surgery. My daughter was furious and called family dr. who wasn’t happy about that decision either. Whether it was begin or not, it doesn’t belong there. I don’t know where you live but don’t stop looking until you find a doctor who will do surgery if it is in an area that can be operated on. In fairness, all the doctors thought it was benign but the rest thought it should be removed. If he hadn’t had surgery he would be dead within a few months of the diagnosis. In a month and a half the tumor first being discovered, it increased in size by half and was about the size of a walnut.
I talked to my oncologist recently about my son-in-law. He said Duke University Hospital (where the BB team is)was the best in the country for brain tumors. My doctor is Dr. Schmotzer in Canton, OH of the Morning Star Cancer Center. He has been designated as one of the top 100 oncologist of the U.S. (not just OH).
I will keep your family in my prayers. I hope this helped at least a little. Keep fighting.
I highly recommend the team at Oregon Health and Science University. Drs Neuwelt and Dr. Cetas.
We looked at the University of Pittsburgh and Johns Hopkins. All facilities are great and up-to-date. Your sister-in-law needs a Tertiary (or teaching hospital). Oh and Denver.
Email me and I will give you more names. Let me know where you live. Also, tertiary hospitals will help with medical expenses and other associated costs.
Janelle
my husband has a recurring stage 2 anaplastic astrocytoma.he was operated on in 2009,then went through 6 weeks of radiation. it came back in jan. of 2013. he went and had gammaknife which is radiation directly to the tumor.it grew back and he was operated on agaion in aug.2013.he has been on temodar since oct. and its still growing.we currently go to forbes hospital in Monroeville pa.his doctor pretty much said theres nothing else he can do. if anyone out there can tell us where we can go next,please email me. thankyou. sharon
Please see post above. also join the Brain Cancer Family on Facebook. There are lots of people there that might have information
Janelle
I have a astrocytoma GII. I found out due to walking and my feet and legs hurt with chronic pain. I was at work and almost passed out. They thought I had MS but after the MRI they found the tumor. They did a brain biopsy in Owensboro KY, then went to Duke University to see Dr. Freeman and sat in a meeting with him and he advised the same thing as Dr. Kevin Ridenhour in Owensboro. Dr. Ridenhour suggested temodar and radiation at the same time. They cannot do surgery because of the location of the tumor. They gave me five years and this Dec will be the end of my five years. It has not grown but I still have many problems due to it. They had me to see another doctor about gamaknife however she told me even though she performs this everyday she would guarantee that I would never walk again. I decided I would not do that right now. So it has not grown but my oncologist has his eye on me, however God has his hand on me and I am a walking miracle. I pray everyone’s journey be filled with positive influence and that you have the best care you possibly can get. I know I have.
My mother was diagnosed in January 2015 with stage 3 astrocytoma. The dr tried to operate but he couldn’t take much of the tumor due to location. since then my mother has done chemo and radiation. she is on the second radiation and we just found out that in 2 months the tumor has grown and another is forming. We are all crushed and the doctors have no answers for us. I am so lost and do not know what to do. I am all my mother has and I am doing the best I can. Her tumor is 5 inches by 8 inches…yes inches not millimeters. we are going to see another dr to try and figure out what we need to do now. She has awful headaches and numbness/weakness on her left side accompanied with memory loss. When she is off chemo she fells good but on chemo its awful. Is it worth doing the chemo if the tumor is still growing? Does anyone have advice for me?
Hopeful daughter
My tumor is inoperable grade two astrocytoma. I flew to Duke University and spoke to Dr. freeman myself and he said he would not touch it. Even though I’m in pain and have some problems I can at least walk and function. Everyone has said if they touched it I would be paralyzed in some form. My tumor sits and is pressed in on my mobility. Even Gama Knife would do the same because of the location. Maybe Dr. Freeman could help you. I’m not sure but they all was so nice. Great place to go.
Christy Im Very Sorry To Hear About Your Mom. Im Not A Doctor. So I Cant Really Tell You What To Do. Just Im Hear For You An Mom. I Have A Astrocytoma Stage 3. To. Ive Had Mine Sence 2002. I Had Surgery But They Couldnt Take It All Out Either. I Get Trouble Headaches. An In Weak Most Of The Time An I Have Numness To. I Don’t Do Chomo / Or Readiation. I Want To Enjoy What Time I Have Lift. I Don’t Want To Bed Stuck In Bed. Now Im Out An Around Doing Things. I Have My Good Days An my Bad Days To. Ill Be Praying For Your Mom. Please Keep In Touch With Me. An Imm let You No How Im Doing Ok. God Bless You Both
My 16 year old son does not have any prior symptom like headache. Last week of Oct 2015, he experienced sudden sharp right headache and sudden weakness of his left body, typical of stroke. Preliminary diagnosis was cavernoma. He went through multiple MRI and pediatric surgeon told us that surgery was necessary due to brain bleed, causing a lot of extreme headaches. Had surgery and diagnosed to have Anaplastic Astrocytoma Stage 2 in the thalamus area. Still experiencing strong headaches and weakness on his left extremities, he can talk though. I am crushed. I don’t know what to do. This is not suppose to be happening to my son full of hope and still very young. Please anybody advise me what to do. He’s my only son, Dr told me he’s going for chemo in combination with radiation therapy. I’m a single mom, and now we are buried with medical bills. Pls, pls advise for other treatments just to prolong my son’s life……
I understand the stress. I am 36 and I was diagnosed with the same when I was 31. I had full brain radiation and chemo for a year. With this together they said worked better. I flew to duke university the largest brain tumor place in the world and spoke to Doc. Freeman and he agreed with the treatment and agreed mine was terminal cancer and inoperable. They gave me five years, and next month will be my five years and I’m still here. Death is no more close to me with cancer then me jumping off a building. I do have problems with my left side of my body, I have a hard time with pain, walking, memory etc. I am still positive and moving on. God only knows my experation date and He gives me the peace and strength I need to face each day. Living with cancer is a struggle not only for me but for my caregiver which is my wife, kids! We do talk about it and anytime they need to cask anything then I’m here to answer with the truth. Just keep a positive outlook be there for him and try not to loose it to much in front of him. Remember he has the cancer , but the cancer don’t have him.
Karen J Wimer has stage three in her left hemisphere. Inoperable. Last night I had to tell her she could choose radiation and maybe chemo or not. It is a large tumor that is deep in her brain . Prognosis is bleak – about four months. Has anyone had any success for a higher survival rate with treatment. I know Duke has a more aggressive surgery program. But how do you get someone to look at existing MRIs and other tests to give a second opinion without having to move the patient to their location? I can’t understand it. I don’t want her to die- but I don’t want her to suffer horribly because I can’t let go or accept the facts . Please respond if you have any information.
I have gone to Duke and I spoke to Dr. Freeman. He is as laid back as your best friend. I was so shocked. He was in a sweatshirt and jeans when we spoke in the big meeting room. I never felt so comfortable talking to someone as him. All my fear left being in a big place and I could ask anything. My oncologist calls him every now and then to discuss my diagnosis. Such an awesome place to go.
Thank you
Karen’s tumor is about half of her left hemisphere and inoperable. Originally seen at the University of Iowa. Talked to Dr. Friedman at Duke and Dr. Rahman at U of Fl. no resecting due to location. a week of radiation left her nearly comatose. Now she is talking and mobile and in hospice. Considering chemo once a month on temador. Prognosis isn’t good. Please pray for her
I sure will. May God himself put a wall of protection around you and his healing hand on you. Prayers being said right now. Be healed in the name of Jesus. Where two or more are in agreement there he will be.
I am not here to BRAG at all. I wanted to tell everyone how blessed I am to still have my Mother. She was diagnosed 16 years ago and still hanging on. She had 33 radiation treatments and 4 years ago a 6 hour radiation treatment. I give all the Glory to God. She first realized she had a tumor, because she was falling a lot and the movement on her left side was failing. When we took her to the Dr. at first the doctors thought she had a Bad STROKE. After a specialist looked at it, A TUMOR! Dr. Kovalic with Jackson General Hospital in Jackson TN was her radiologist. Mom gradually lost her ability to walk. She is 79 and has been in the Nursing Home 3 years. She still knows us all and although she can’t do things like she once did, I am so thankful she still knows us all and we can visit. She was given 2-3 years to live. Blessings and Prayers to You all!
God Bless Your Mom An Family. She Sounds Like A Very Sweet Lady. I Hope You Have Her Here With Youle For Many years To Come. Ill Keep Praying For Her .I Have Cancer Of The Brain To Sence 2002.My Tumors Affecting My Eye Sight This Time Around.They Cant Operate Anymore. I’m Not Having Chimo/Or Radiation.Im Still Here. Its 2016 Now But My Headaches Are Getting Bad Again. An The Tumor Is Growing Back Again. Well Mom. You Keep Smiling. God Loves You An So Do I.