What is ovarian teratoma?
Ovarian teratoma is a benign or malignant tumor belonging to a group of germ cell tumors. It develops from germ cells and can be composed of different cell types from all the germ layers. It is also referred to as dermoid cyst, although this name only is used for benign neoplasm. Three layers of germ cells- ectoderm, mesoderm and endoderm are formed early in the embryonic period.
From these cell layers all the tissues are formed. Germ cell is an embryonic cell that can develop into gamete- cell containing 23 chromosomes that unites with the opposite sex germ cell can form an embryo. Germ cells are totipotential- that means they can develop into any type of cells [1].
Types
In literature usually two types of ovarian teratomas are distinguished:
Benign
Well differentiated, mature cystic lesion. This is the most common type of ovarian germ cell tumor. It is usually diagnosed in woman during reproductive years (between 12 to 45 years of age)
Malignant
Solid, poorly differentiated tumors. This type of tumor is usually present in woman under 20 years of age and it is extremely rare.
Another type of ovarian teratoma is monodermal teratoma. It contains cells from only one type of tissue. There are 3 types of monodermal teratomas:
- Struma ovarii
- Carcinoid tumors
- Neural tumors[1,4]
Causes
It has been discovered that teratomas arise from a single germ cell after its first division. By using sophisticated molecular techniques and genetic testing, scientist suggested the parthenogenic theory. This theory suggests that tumors are anatomically distributed along the migration patterns of primordial germ cells [4].
Mature cystic teratoma
Clinical presentation
Mature cystic teratoma is a benign neoplasm that is composed of tissue from at least two germ cell layers (also read: solitary fibrous tumor). Although they might be present at any age, most commonly this type of teratoma is seen in young woman (around 30 years of age).
Mature cystic teratoma is usually asymptomatic. If the teratoma is bigger in size, it can cause some unspecific symptoms like abdominal discomfort or pain. These teratomas grow slowly, approximately 2 mm each year. In around 10% of cases they affect both ovaries [2].
Pathology
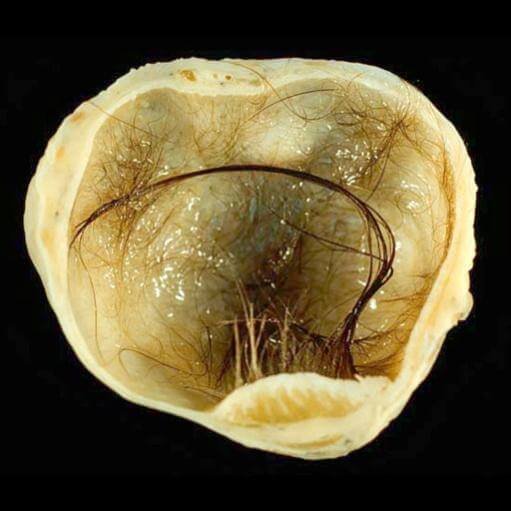
These teratomas are usually present in one place. They are filled with semi-solid liquid and tissues that lie within the wall. Sometimes tissue like hair follicles, skin glands, nails and even mature teeth can be found. The walls of the cyst are lined with squamous cells. Usually there is a nodule in the cavity, called Rokitansky nodule. In this nodule usually teeth and bone are located. In majority of cases fat, bone, cartilage, gastrointestinal and bronchial tissue are seen[2].
Diagnosis
There are no specific laboratory studies for mature cystic teratomas. Usually the diagnosis can be made using imaging studies:
- Ultrasound is the most common method used for diagnostics. It can be complicated due to different presentation of the tumor. Usually a cystic lesion with dens nodule in the lumen can be seen. The ultrasound appearance varies depending on the contents of the cyst.
- CT imaging can show calcifications in the wall of the cyst. Sometimes hair mass can be determined if the surrounding fluid is full of fat.
- MR imaging is sensitive for cysts on T1 weighted images due to the fat component of the cyst. Fat-sensitive sequence can also help to differentiate this type of cyst from a hemorrhagic lesion [2].
 Treatment
Treatment
Mature cystic teratomas can be surgically removed and they don’t require any other treatment [5].
Complications
- Rupture- causes the leakage of sebaceous fluid in the abdominal cavity, which can lead to peritonitis
- Torsion- can cause loss of blood flow to the cyst and enlargement of the cyst, which can lead to rupture.
- Malignant degeneration of the cyst can lead to:
- Carcinoma- squamous cell carcinoma is the most common type of malignant degeneration
- Sarcoma(also see uterine sarcoma)[2]
Immature teratoma
Clinical presentation
Immature teratomas are also made of at least two germ cell layers. This type of tumor affects younger patients (until the age of 20 years). These teratomas are often seen in combination with mature teratomas. In around 26% cases there is also a mature teratoma in the same ovary, and in around 10% on the opposite side [3].
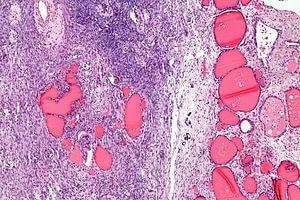
Pathology
Immature teratomas are around 14-25 cm large, solid or with cystic component. The cystic part can be filled with mucinous or fatty-sebaceous fluid. The tumor staging is based on the amount of tissue present. Another staging and grading predictor is α-fetoprotein[3,4].

 Diagnosis
Diagnosis
A certain diagnosis can only be made after histological examination of the teratoma. Other methods can be used to help distinguishing it from other conditions:
- Ultrasound imaging is not specific. Usually a solid or cystic-solid tumor can be seen. Calcifications might be present.
- CT and MRI- large, solid tumor with irregular shape can be seen. Calcifications are scattered. Bleeding can often be seen[3,4].
Staging
The stages of immature teratoma represent its growth. It is a prognostic feature to help determine the necessary treatment plan and possible outcome.
- Stage I- tumor does not expand outside the ovary
- Stage II- tumor has spread in the pelvic organs
- Stage III- tumor has spread to regional lymph nodes or peritoneum
- Stage IV- tumor has metastasized to other organs (also see staging of Fallopian tube cancer)
Grading of the tumor is also important to determine the outcome. Grade describes the maturity of the tumor cells. If cells are poorly developed and grow faster, the higher the tumor is graded [5].
Treatment
The treatment of choice is surgery. In stage I tumors, where the tumor has not spread outside of the ovary, surgery is usually very successful. Still, the recurrence rate is high- for first stage cancer it is 18%, but stage for- even up to 78%. [6] In other cases chemotherapy is used as an adjuvant therapy. When treated with chemotherapy, these neoplasms can undergo retroconversion- a process when immature teratoma starts to look like mature cystic teratoma[5].
Monodermal teratomas
This type of teratoma is usually composed from one type of tissue:
- Struma ovarii – teratoma that is composed of thyroid tissue. This type of teratoma is usually benign, but in some cases it can cause thyriotoxicosis.
 Carcinoid tumor – solid tumors, usually seen in postmenopausal women. This type of teratoma is benign, but it has a potential to be malignant.
Carcinoid tumor – solid tumors, usually seen in postmenopausal women. This type of teratoma is benign, but it has a potential to be malignant.- Neural tumor – neural tissue can form both benign and malignant tumors, for example neuroectodermal tumor that is very aggressive[4].
Support ovarian cancer by wearing teal ribbon.
If you found this article helpful, share it to others on social media. For your personal experience use the comments box below.
References
- Patient information: http://www.medicinenet.com/script/main/art.asp?articlekey=4703
- Mature cystic teratoma: http://emedicine.medscape.com/article/281850-treatment
- Immature teratoma: https://radiopaedia.org/articles/immature-ovarian-teratoma
- Detailed information for health professionals: http://pubs.rsna.org/doi/full/10.1148/radiographics.21.2.g01mr09475
- Treatment of teratomas: http://www.cancerresearchuk.org/about-cancer/cancers-in-general/cancer-questions/what-is-teratoma-of-the-ovary
- Prognosis: https://www.cancer.gov/types/ovarian/hp/ovarian-germ-cell-treatment-pdq
Similar Posts:
- Germ Cell Cancer – Symptoms, Survival Rate & Prognosis
- Serous Cystadenoma
- Brenner Tumor
- Pineal Gland Tumor
- Childhood Leukemia
- Choriocarcinoma – Symptoms, Prognosis, Treatment, Diagnosis
- Syringoma – Treatment, Removal, Pictures, Causes, Surgery, Prevention






Leave a Reply