What is Parotid Gland Tumor?
Pleomorphic adenoma is the most common benign parotid growths accounting for 80% of cases, followed by Warthin’s tumor, covering about 6- 10% of cases.

Parotid malignancies are less common and these include mucoepidermoid carcinoma, adenocarcinoma, mixed malignant tumors and squamous cell carcinoma. Benign growths typically occurs after age 40 with higher incidence among women, whilst malignancy presents after age 60 with equal distribution in both genders.
Benign tumors particularly pleomorphic adenomas, can transform into malignant mass called carcinoma ex-pleomorphic adenoma. The malignant transformation leads to sudden rapid unstable growth of the tumor which are more aggressive with poor prognosis.
Symptoms
Parotid Gland Tumor is more common in the distal portion of the gland presenting as a discrete mass. The abnormal growth typically presents as slow-growing, solitary, unfixed neoplasm in the parotid area, although some are multinodular and fixed. Symptoms in most patients occur in a duration of less than a year up to several decades.
Pain or discomfort, which is often intermittent and vague, is experienced in malignant as well as benign masses. This results from bleeding or suppuration into a lesion or due to infiltration of nearby tissues.
Clinical presentations suggestive of malignancy upon deep palpation of the parotid tumor include: hard, non-movable tender mass, overlying ulceration and infiltration of adjacent structures like lymph nodes and facial nerve. Facial paralysis indicates malignancy.
Ultrasound is the most common early diagnostic procedure indicated to determine superficial lesions. Fine needle aspiration (FNA) guided by ultrasound is performed to obtain samples for cytological examination. CT scan guided biopsy can also be employed as an alternative means for cytology.
After confirmation, CT scan or MRI is indicated to evaluate tumor mass and spread to nearby areas or specific organs. The staging of lesions in malignant parotid cases is based on the commonly used tumor, node and metastasis (TNM) system which correlates with patient’s survival and actual management.
Causes
The human parotid gland is divided into serous lobules with significant adipose tissues by a fibrous layer. It contains lymph node tissues and lymphoid aggregates which contain ducts of the salivary gland. Parotid is one of the major salivary glands where 80% of salivary neoplasms develop.
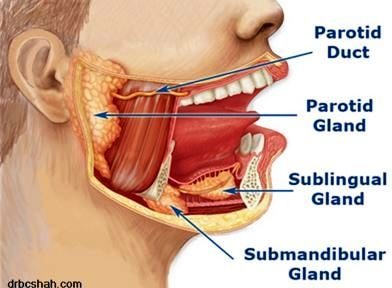
Image 2 – Location of Parotid Location
The exact etiology of parotid tumors remain unknown, however, several contributory factors are established. Genetic predisposition could be related to monosomy and polysomy, structural genetic alterations and allelic loss. Neck radiation exposure has been associated with parotid and other salivary glands malignancies.
Smoking is significantly related to Warthin’s tumors which increases the risk by eight fold compared to non-smokers. Rampant use of mobile phones remains a controversial risk factor in the development of both benign and malignant neoplasm of the parotid gland.
Treatment
Parotid gland tumor is typically initially managed with ablation therapy. Radiation therapy is indicated after surgery especially for high-grade lesions and non-resectable tumors. Radiotherapy improves the overall survival rate of patients as an adjunct management to surgery.
This therapy utilizes high-energy x-rays to kill or control tissue growth. Special radiation types may include fast neutron radiation therapy, which uses invisible neutron particles, and photon-beam radiation therapy which reaches deep tumors with the use of linear accelerator machine.
Polychemotherapy is commonly used for palliative regimen of advanced conditions which are no longer responsive to local therapies of surgery and radiotherapy. Oral mucositis and dryness of the mouth or xerostomia may be experienced after radiation therapy.
Surgery (removal)
Benign parotid neoplasms require excision of the gland. Superficial parotidectomy with facial nerve dissection may be indicated for the treatment of parotid growth. If malignancy is established, more radical procedure will be required with the severance of the facial nerve and complete excisions of the gland.
Complications related to surgical management need to be monitored in the perioperative period. The facial nerve may be damaged or paralyzed due to infiltration of parotid tumor or surgical procedure. Recurrence of the tumors have also been reported, hence tumors like pleomorphic adenomas need to be completely removed.
Recurrence is usually multifocal which can occur after 10 to 15 years with significantly decreased cure rate. Freye’s syndrome, which is characterized by erythema and sweating of the cheek during eating, chewing, thinking of seeing food that stimulates strong salivation, can develop in the postoperative period. This is brought about by abnormal reformation of autonomic nerves which results to facial sweating with salivation stimulus.

Image 3 – Before Vs after Surgical resection of Parotid Gland
Pictures

References
Barnes, L., Eveson, J., Reichart, P. and Sidransky, D. (eds) (2005). WHO classification of tumors: Pathology and genetics head and neck tumors. International Agency for Research on Cancer (IARC) Press, Geneva, Switzerland. 208-281.Retrieved from www.iarc.fr/IARCPress/pdfs/index1.php
Davis, C. (2011). Salivary gland cancer facts. Medicinenet.com. Retrieved from http://www.medicinenet.com/salivary_gland_cancer/article.htm
Hatch, R. and Shan, S. (2005). Warthin tumor: a common, benign tumor presenting as a highly suspicious mass. JABFP. 18 (4):320-322.
National Cancer Institute (2012). PDQ Salivary Gland Cancer Treatment. Bethesda, Md: National Cancer Institute. Retrieved from http://cancer.gov/cancertopics/pdq/treatment/salivarygland/HealthProfessional.
National Cancer Institute (2011). Salivary Gland Cancer Treatment. (PDQ®). NIH: National Institutes of Health. Retrieved from http://www.cancer.gov/cancertopics/pdq/treatment/salivarygland/Patient
National Comprehensive Cancer Network. (2013) Clinical Practice Guidelines in Oncology (NCCN Guidelines): Head and neck cancers. NCCN: National Comprehensive Cancer Network Version 2. Retrieved from http://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf.
Patient (2015). Salivary gland tumours. Patient. Egton Medical Information Systems Limited, England. Retrieved from http://www.patient.co.uk/doctor/salivary-gland-tumours
Sadetzki, S., Oberman, B., and Maldelzweig, L., et al. (2008). Smoking and risk of parotid gland tumors: a nationwide case control-study. Cancer. 112 (9): 1974-82.
Schiff, B. (2015). Salivary gland tumors. Merck Sharp & Dohme Corp, NJ, USA. Retrieved from http://www.merckmanuals.com/professional/ear-nose-and-throat-disorders/tumors-of-the-head-and-neck/salivary-gland-tumors
Similar Posts:
- Acinic Cell Carcinoma
- Pituitary Gland Tumor
- Pineal Gland Tumor
- Nerve Sheath Tumor
- Solitary Fibrous Tumor
- Pineoblastoma
- Neuroblastoma






Leave a Reply