Definition
Insulin is the hormone that is accountable for managing the body’s amount of sugar in the blood. This hormone also helps glucose to transfer into body cells from the blood. Insulinomas produce insulin.
Insulinomas are benign or non-cancerous tumors of the pancreas that rarely occurs to individuals and produces too much amounts of insulin. Blood sugar normally rises when a person eats which directs the pancreas to increase its insulin production.
The pancreas will only stop making insulin if the blood sugar has returned back to normal levels. When an individual has an insulinoma tumor, the growth will keep on producing insulin. This indicates that the blood sugar level will continuously drop which could result to seriously low levels of blood sugar.
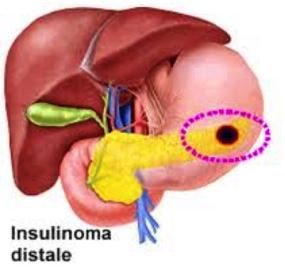
They are composed of specialized beta islet cells that secrete insulin from time to time, causing low blood sugar. These tumors usually grow slowly and could arise in any area of the pancreas. Women are more prone to these tumors rather than men. The tumors are approximately 2cm and an overall percentage of 90% of individuals have benign insulinomas and the remaining 10% are malignant.
Symptoms of Insulinoma
Individuals with insulinomas do not always have obvious symptoms. Slightly low blood sugar symptoms are frequently ignored or sometimes mistaken for other conditions.
People might live their lives for several decades without being diagnosed. Other severe symptoms of the tumor can affect the brain and the adrenal glands.
These glands manage the heart rate and stress response. Some symptoms are much the same to those of epilepsy. Epilepsy is a type of neurological condition that causes seizures.
Mild symptoms involve:
- Shakiness
- Confusion or forgetfulness
- Sweating
- Blurred or doubled vision
- Gaining of weight
- Anxiety
- Lightheadedness
- Hunger
- Abnormal behaviors
More severe symptoms might include:
- Amnesia
- Seizures
- Fast heart beat or pounding of the heart
- Coma or loss of consciousness
In some cases, tumors can grow larger or metastasize. These symptoms may involve:
- Jaundice or the yellowish discoloration of the skin and eyes
- Pain in the abdomen
- Diarrhea
- Back pain
Causes
Scientists do not know the reason why individuals get insulinomas. The growths usually show up with no warnings. The sudden appearance of an insulinoma can change the management of glucose and could result to hypoglycemia.
An insulinoma is a neuroendocrine tumor that is primarily obtained from pancreatic islet cells. About 10% of individuals with malignant tumors have a unique family syndrome which could either be multiple endocrine neoplasia type 1 (MEN 1) or von Hippel-Landau syndrome. Approximately 21% of patients with MEN 1 have insulinomas.
Diagnosis
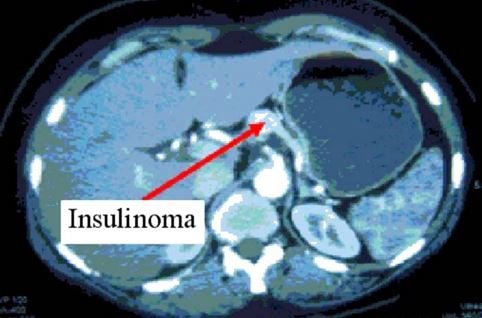
The diagnosis of insulinomas involves the simultaneous measurement of insulin levels and blood sugar in the blood. If the person has a high insulin level and a low blood sugar, then insulinoma is confirmed. Once the diagnosis is totally made based on the biochemical analysis, the physician will execute further studies to find the pancreatic tumor.
Tests may include:
Computed tomography/CT scan
It is an imaging test that can produce cross-sectional images of the body to help the physician find the tumor.
Magnetic resonance imaging/MRI scan
It is an imaging test that could show images of structures and organs inside the body to locate the tumor.
Ocreotide scan
It is a kind of scintigraphy that could detect pancreatic neuroendocrine tumors.
Endoscopic ultrasound
This is used if the tumor cannot be seen with standard scans. The test takes pictures inside the body with the use of sound waves. The location of the tumor will be specified and a biopsy can also be taken through this test. It could help the physician distinguish whether the tumor is malignant or not.
Treatment
The primary treatment for insulinomas is surgery since the symptoms of approximately 90% of patients are cured from tumor removal. Most cases of patients will not require further treatments after the tumor has been removed.
The procedures that are commonly performed for the removal of insulinoma include:
Pancreatic resection
Sometimes the surgeon might remove some part of the pancreas where the tumor is situated through a whipple operation or distal pancreatectomy. These operations are only performed if needed depending on the physician’s evaluation.
Enucleation
The surgeon only removes the tumor itself without touching the rest of the pancreas. The recurrence rate after the procedure is very low. However, it still depends on the patient’s health status.
Laparoscopic surgery
If one small pancreatic tumor is present, it will be removed through this procedure. It is a minimally invasive surgery that only requires a small incision.
Chemotherapy
It is a procedure that could help control the symptoms of a cancerous tumor that cannot be removed with surgery. The drugs that may be used are streptozocin and doxorubicin.
Cryotherapy
It is a therapy that can treat malignant tumors with the use of low temperatures. It could destroy abnormal tissues by freezing it.
References
- http://www.cancerresearchuk.org/about-cancer/cancers-in-general/cancer-questions/insulinomas#Tests
- http://www.surgery.usc.edu/divisions/tumor/pancreasdiseases/web%20pages/Endocrine%20tumors/pancreatic%20tumors/insulinoma.html
- http://www.healthline.com/health/insulinoma#Treatments6
- Guettier JM, Lungu A, Goodling A, Cochran C, Gorden P (2013 Sep 30). The Role of Proinsulin and Insulin in the Diagnosis of Insulinoma: A Critical Evaluation of the Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab.
- Mathur A, Gorden P, Libutti SK (2009 Oct). Insulinoma. Surg Clin North Am. 89(5):1105-21.
- Begu-Le Corroller A, Valero R, Moutardier V, Henry JF, Le Treut YP, Gueydan M (2008 Jun 13). Aggressive multimodal therapy of sporadic malignant insulinoma can improve survival: A retrospective 35-year study of 12 patients. Diabetes Metab.
Similar Posts:
- Neuroendocrine Cancer – Symptoms, Treatment, Prognosis, Survival Rate
- Serous Cystadenoma
- Stage 4 Pancreatic Cancer – Symptoms, Survival Rate, Life expectancy
- Vipoma
- CEA Tumor Marker
- Duodenal Cancer – Symptoms, Prognosis, Survival Rate and Treatment
- Link Between Low Testosterone and Testosterone Replacement Therapy on Cancer






Leave a Reply