Definition
Craniopharyngiomas are benign or noncancerous rare tumors which mean that they do not aggressively spread to other parts of the body and brain. They are nearly situated between the pituitary gland and the hypothalamus. (The pituitary gland is the pea-sized organ located at the bottom of the brain and controls other glands, while hypothalamus is the organ that is connected to the pituitary glands.)
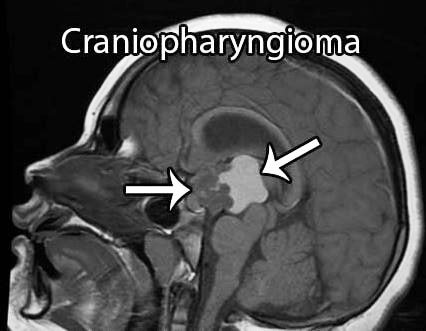
These tumors are characterized as partly-fluid and partly solid mass, and could press and grow on some nearby locations such as the optic nerves, pituitary gland, fluid-filled spaces of the brain, and the optic chiasm. The condition can affect numerous of brain functions like vision, hormone production, and growth.
This is accountable for 2-4% of predominant brain tumors which usually affects children, but could also affect adults with ages 50 years old and above. These tumors are correlated with Rathke’s cleft cyst which is also a non-cancerous tumor located in the pituitary gland, particularly a fluid-filled cyst positioned in the anterior pituitary gland on the posterior portion.
Symptoms of Craniopharyngioma
The symptoms of craniopharyngiomas depend on the location of the tumors:
- The vision decreases as caused by an optic nerve damage that are frequently permanent or progresses and gets worse after a surgical operation to remove the tumor.
- When the pressure on the brain increases, the person will experience nausea, vomiting, headache, and will have trouble on balancing.
- Once the pituitary gland becomes defective, hormonal imbalances will occur resulting to slowed growth, fatigue, low blood pressure, constipation, immoderate urination, menstrual issues, and excessive thirst.
- Learning and behavioral problems might also be present.
- If the hypothalamus is affected, it might lead to diabetes insipidus, obesity, and drowsiness.
Causes of Craniopharyngioma
Craniopharyngiomas typically affects children between 5 to 14 years old. As a matter of fact, 50% of patients with this disease are under 18 years old. Both genders are equally prone to the development of this condition.
However, the causes of the tumors are still unknown, but they do not occur to run in families or are genetically inherited from parents.
Diagnosis
The diagnosis of craniopharyngiomas are commonly made in accordance to radiology studies like:
Magnetic resonance imaging or MRI scan of the brain with the gadolinium substance injected into a vein. MRI scans can produce brighter images of the tumor cells which are very helpful for the diagnosis. Since the condition is benign, no additional scans are usually needed unless the physician requires.
Other tests and procedures are also possible such as:
- Physical examination and medical history of the patients will be taken.
- To check a patient’s coordination, mental status, and reflexes, a neurological or neuro-exam is done to assess the function of the nerve, spinal cord, and brain.
- A visual field exam may be proposed to measure the patient’s peripheral and central vision. Any vision loss can possibly indicate that there is a tumor present that caused some damage on certain parts of the brain in which the eyesight gets affected.
- A CT (computed tomography) scan may be performed to see detailed images of the body from different angles.
- Blood chemistry studies wherein a patient’s blood sample is studied for any signs of the disease
- Blood hormone studies to measure some hormones set into the blood by body organs and tissues.
Treatment
Surgery
The primary treatment for craniopharyngiomas is typically surgery and the goal is to totally remove the tumor while enhancing or preserving the brain, pituitary, and visual function.
Craniotomy
A craniotomy is preferred when the tumor is above the suprasellar tumors in order to remove it and for optical exposure.
Transsphenoidal route
For patients with relatively small tumors cited in the pituitary gland, a transsphenoidal route may be used.
Radiation treatment
Radiation treatment is recommended if the tumor cannot be removed completely to control the growth and prolong the lifespan of the patient.
Stereotactic and conventional radiosurgeries
Stereotactic and conventional radiosurgeries are potent in managing the tumors, but stereotactic radiosurgery provides a safer dose of higher radiation. As a result, radiation techniques are much preferable but since the tumors can still come back after several years from radiation treatment, all patients cured with radiation must have an evaluation at fixed intervals by an endocrinologist for the rest of their lives.
Computed tomography scan and Magnetic resonance imaging
CT scans and MRIs might be repeatedly needed at least once in a year for the first few years after radiation therapy or surgery.
Prognosis
Generally, the prognosis for craniopharyngioma patients is good. Approximately 80% to 90% chance of the patient achieve permanent cure if the tumor has been removed completely through surgical treatments or high doses of radiation.
There is a probability that the disease will recur but it will commonly return within the first two years from surgery. Each patient’s prognosis depend on some factors such as age, size of the tumor, treatment side effects, location of the tumor, recurrence, and whether there are still some tumor cells present even after surgery.
References
- craniopharyngioma – symptoms, diagnosis, treatment at https://pituitary.org/knowledge-base/disorders/craniopharyngioma
- http://www.cancer.gov/types/brain/patient/child-cranio-treatment-pdq
- Craniopharyngioma – Causes, Symptoms, Exams, Prognosis at https://www.nlm.nih.gov/medlineplus/ency/article/000345.htm
- Müller HL (2014). Craniopharyngioma. Handb Clin Neurol. 124:235-53.
- Jung TY, Jung S, Jang WY, Moon KS, Kim IY, Kang SS (2011 Nov 21). Operative outcomes and adjuvant treatment of purely third ventricle craniopharyngioma after a transcallosal approach. Br J Neurosurg.
- Stamm AC, Vellutini E, Balsalobre L. Craniopharyngioma (2011 Aug). Otolaryngol Clin North Am. 44(4):937-52, viii.
Similar Posts:
- Pituitary Gland Tumor
- Pineal Gland Tumor
- Inoperable Brain Tumor
- Pineoblastoma
- Link Between Low Testosterone and Testosterone Replacement Therapy on Cancer
- Retinoblastoma
- Glioblastoma Multiforme – Life Expectancy, Stage 4, Survival Rate, Symptoms, Prognosis






Leave a Reply