Gestational Trophoblastic Disease Definition
Gestational trophoblastic disease abbreviated as GTD is the name used for certain tumors that rarely occur in times of pregnancy in the outer area of the sac referred to as fetal chorion, where it surrounds the baby in the womb as it grows.
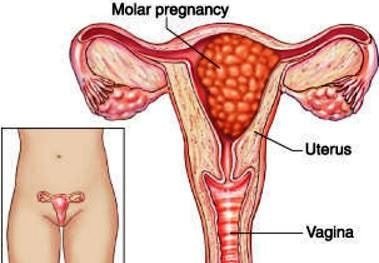
Image 1 – Molar Pregnancy
This tumor starts to grow when trophoblast cells; the placenta’s normal cells, changes and form a mass. The condition is usually benign or non-cancerous in most cases although some growths can be malignant, which means they could proliferate to other body parts. Gestational Trophoblastic Disease commonly occurs when there is some problem in the combination of a woman’s egg and a man’s sperm.
The placenta is the organ that is developed in the course of the pregnancy, so that the mother can supply enough nutrients to the fetus. Trophoblast cells aids in the formation of the placenta by connecting the fertilized egg to the uterine wall. When this problem occurs, a tumor is formed instead of a healthy fetus.
Symptoms
It is essential that the woman talks to the physician if any abnormal symptoms occur during pregnancy since GTD might be suspected based on its common pattern of signs and symptoms.
Gestational Trophoblastic Disease does not normally cause symptoms in early stages since it may be similar to a woman’s normal pregnancy.
Symptoms that could indicate a potential problem include:
- Bleeding of the vagina throughout or after pregnancy
- Weight loss
- Anemia which is the low count of blood cells that could cause breathing problems, dizziness, an uneven heartbeat, and fatigue
- A bigger uterus than the expected in the pregnancy
- Severe sweating or shakiness
- Pain in the pelvic area
- Sleeping problems
- Abdominal swelling
- Anxiety
- A pregnancy wherein the movement of the baby has not changed at the expected time
- High blood pressure that may be accompanied with hands and feet edematous and/or headaches
- Severe vomiting and nausea in times of pregnancy
Causes & Pathology
The egg cells and sperm will normally produce a set of 23 chromosomes and creating a cell with a total of 46 chromosomes. The cell will then divide and will become a fetus after some time. This normal process does not happen with Gestational Trophoblastic Disease.
Complete hydatidiform mole is a type of GTD with an abnormal egg cell that has no chromosomes is fertilized by a sperm cell. The reason why the egg has no chromosomes is unknown. When this occurs, no fetus is formed but rather, a complete hydatidiform mole develops.
Partial hydatidiform mole is a hydatidiform mole mass that rarely develops inside the uterus at the start of pregnancy.
This occurs when a single normal egg cell is fertilized by 2 sperm cells at the same time, which will then result to 69 chromosomes instead of 46. An embryo with a total of 69 chromosomes cannot grow and develop into a normal infant but instead, a malformed fetus with a partial hydatidiform mole and normal placental tissue is formed.
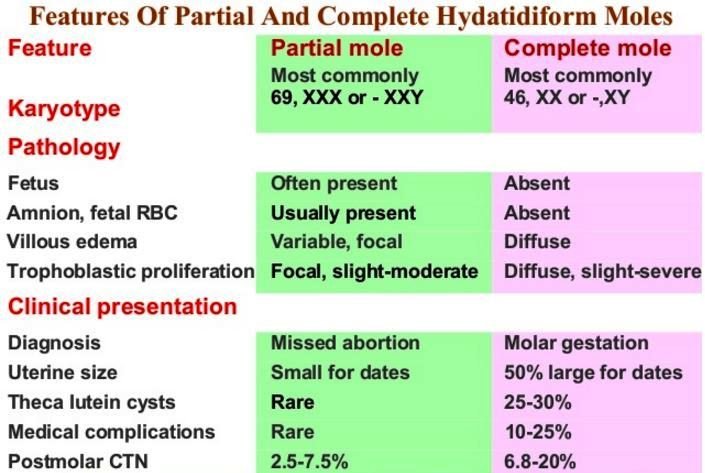
Image 2 – GTN – Complete Vs Partial Mole
Choriocarcinomas mostly develop from recurring hydatidiform moles and when some tissues are left in the womb after an abortion, miscarriage, or the delivery of the baby. Certain changes in the genes cited in choriocarcinoma cells have been found by researchers, but are not clear as to what causes it.
Invasive moles are hydatidiform moles that grow in the uterine muscle layers. The causes are not clear as to why it happen.
Placental-site trophoblastic tumor (PSTT) usually develops after full-term pregnancies and they do not have any villi compared to the other moles.
Epithelioid trophoblastic tumors are very rare tumors which also develop after full-term pregnancies though it could occur many years later.
Diagnosis
Diagnostic procedures involve:
Ultrasonography
This is very important in the diagnosis of Gestational Trophoblastic Disease in order to view the internal structures of the body. An ultrasonographic pattern may be noticed which consists of various holes in the placental mass and no fetus are usually present. Focal cystic spaces in the placenta may also be demonstrated in this diagnosis.
Blood or urine tests
Elevated human chorionic gonadotropin (hCG) hormone is revealed in blood or urine tests. If hCG is elevated, it should also be measured since GTD is suspected.
Treatment
Treating Gestational Trophoblastic Disease usually involves evacuation of pregnancy and other procedures to prevent complications and ease symptoms. Treatment options for this disease include:
Chemotherapy
This is very effective in treating GTD. It involves the use of anti-cancer drugs for cancer cells that had already spread to other areas of the body.
Suction curettage
This is for the removal of uterine contents from the cervix.
Hysterectomy
This refers to the surgical removal of the uterus and other surrounding affected structures.
Radiotherapy
This is only used if the cancer has spread and the patient is not responding to chemotherapy. The said treatment utilizes uses high-energy x-rays to disrupt cancer cells.
Complications
The disease can cause an extensive range of complications and this includes:
- Ovarian cysts
- Excessive production of thyroid hormone
- Hemorrhage
- Shortness of breath
- Pre-eclampsia in which certain substances in the blood are high
- Gestational Trophoblastic Disease that keeps recurring
Pictures
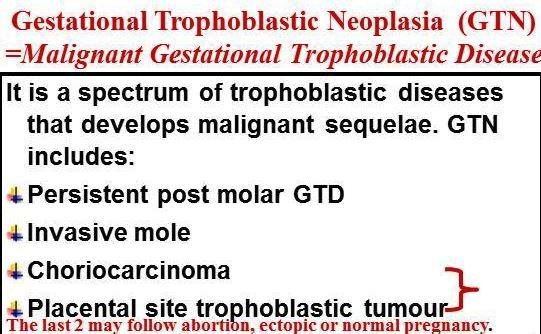
Image 2 – GTN Types
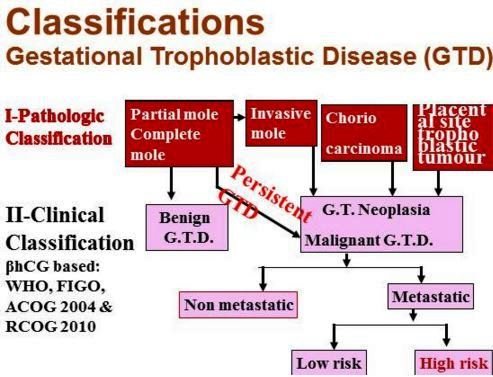
Image 4 – Gestational Trophoblastic Disease Pathological and Clinical Classification
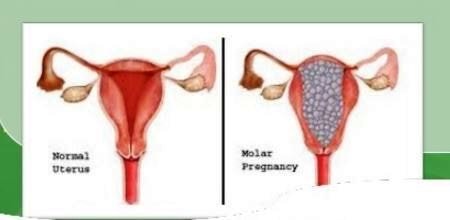
Image 5 – Normal uterus vs molar pregnancy
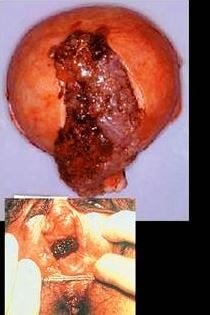
Image 6 – Gestational trophoblastic disease image
References
- Overview, Statistics, Medical Illustrations,Risk Factors, Symptoms and Signs, Diagnosis, Stages and Groups, Treatment Options, About Clinical Trials, Latest Research Coping with Side Effects After Treatment at at http://www.cancer.net/cancer-types/gestational-trophoblastic-disease
- http://www.ajog.org/article/S0002-9378(10)00853-7/fulltext#sec6.1
- http://www.cancer.org/cancer/gestationaltrophoblasticdisease/
- Seckl MJ, Sebire NJ, Fisher RA, et al (2013 Sep 1). Gestational trophoblastic disease: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol.
- Osborne R, Filiaci V, Schink J, et al (2008). A randomized phase III trial comparing weekly parenteral methotrexate and “pulsed” dactinomycin as primary management for low-risk gestational trophoblastic neoplasia: A Gynecologic Oncology Group study. Gynecol Oncol. 108:S2-S3.
- Chakrabarti BK, Mondal NR, Chatterjee T (2006 Nov). Gestational trophoblastic tumor at a tertiary level cancer center: a retrospective study. J Reprod Med. 51(11):875-8.
Similar Posts:
- Partial Molar Pregnancy – Pictures, Symptoms, Treatment
- Choriocarcinoma – Symptoms, Prognosis, Treatment, Diagnosis
- Fibroid Tumor
- Cervical Intraepithelial Neoplasia
- Childhood Leukemia
- Chronic Myelogenous Leukemia
- Chronic Lymphocytic Leukemia






Leave a Reply