Ependymoma Definition
The brain is the organ which is accountable in controlling vital functions like senses, memory, and learning. The spinal cord is composed of nerve fibers that link the brain in the nerves of certain body parts. Ependymoma is a rare tumor that arises from ependymal cells lining the ventricles and passageways in the spinal cord and brain.
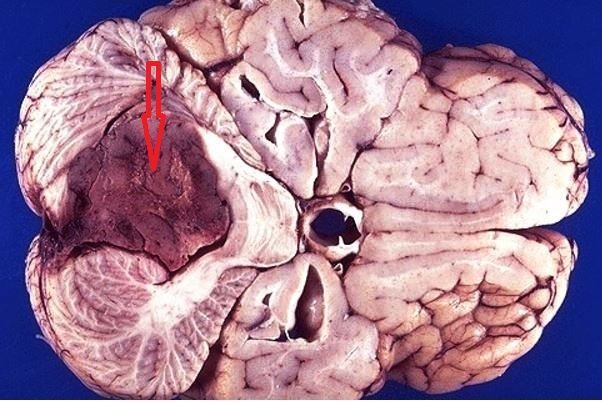
These cells also produce cerebrospinal fluid (CSF). Ependymomas are soft, red, or grayish in color that may possibly comprise of mineral or cysts calcifications.
They can occur in both children and adults. The tumors do not grow fast and does not affect body systems; instead they just displace its growth somewhere else within the central nervous system.
Ependymomas are classified into four types:
Subependymoma (grade I)
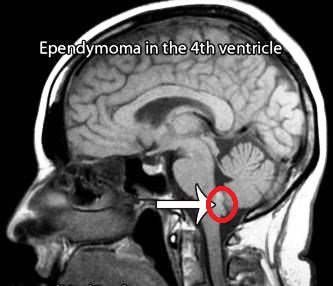
This type of ependymal tumor is commonly found in the fourth ventricle, but could occur anywhere else where ependyma is present. This does not usually occur in children.
Ependymomas (grade II)
These tumors can be seen somewhere next or within the ventricular system and can be divided further into subtypes; cellular ependymomas, papillary ependymomas, tancytic ependymomas, and clear cell ependymomas.
Myxopapillary ependymomas (grade I)
These tumors have slow restricted growths on a specific site and they usually occur in the lower area of the spine called filum terminale. Children are not commonly affected.
Anaplastic ependymomas (grade III)
These tumors have faster growth rates compared to the others and have poorer prognosis. These tumors are typically cited in the lower back area of the skull in children and in the brain for adults. It is not common that they are found in the spinal cord. However, there are still disputes and doubts concerning the microscopic characteristics in anaplastic ependymomas from classic ependymomas.
Symptoms of Ependymoma
The signs and symptoms of ependymomas vary accordingly on the location of the tumor and the age of the patient. The tumors are commonly seen in three major locations:
- Posterior fossa – the area of the brain that contains the brainstem and the cerebellum
- Spinal cord
- Supratentorium – the part of the brain that contains the cerebral hemispheres
Tumors in the posterior fossa symptoms:
- Vomiting
- Headaches
- Nausea
- Blurred or doubled vision
- Head tilt
Tumors in the spinal cord symptoms:
- Back pain
- Scoliosis
- Sciatica
- Different leg lengths
- Extremity weakness
Symptoms of those tumors that occur somewhere on the fourth ventricle:
- Wry neck that is accompanied with a tilted and twisted head
- Loss of stability or walking difficulties
- Weakened or damaged hearing
- Difficulty of speech articulations
- Swallowing problems
- Dysmetria or the body’s lack of coordination of movement
Causes
The underlying causes of ependymomas are still not known and require more study. According to traditions, ependymomas are observed to come about from oncogenetic events that change the ependymal cells into tumor phenotypes.
These genetic events are uncertain. Nevertheless, there are some progress that had been made in describing the mutations that segregate with other tumor phenotypes. Some information now indicates as a proof that radial glia could be the cells of origin.
Diagnosis
The diagnosis of ependymomas can be done through:
CT scan
This provides images of the brain in order for the physician to get any findings about the tumors
MRI
This also provides images of certain body parts or organs that is much preferred since there is no radiation exposure
Biopsy
If a brain tumor is present, a biopsy may be done to remove a brain tissue sample in order for the pathologist to study the tissue under a microscope and look for any possible cancer cells
Spine MRI
This is for the assessment of the patient’s spinal anatomy
Treatment
Factors such as grade and location of the tumor and the patient’s age should first be considered before deciding about the treatment.
Surgery is the initial treatment option for ependymoma in which the neurosurgeon will aim to possibly remove as much tumor without causing any damage to the brain, which might result to permanent neurological deficits.
Radiation therapy is commonly recommended for children after recovering from a surgical treatment.
Chemotherapy treatment is unclear for ependymomas although in some cases, it is used to treat tumors that recurred after radiation therapy, or to detain radiation in children who are too young and in infants.
Prognosis
The prognosis of a patient will depend on the surgical resection of the tumor. If the tumor is totally removed, the prognosis is better.
Younger patients, specifically those who are 4 years old and below have a worse prognosis mainly because they have a higher chance of developing high grade ependymomas, delays in radiation therapy procedure, and the lateral posterior fossa position of the tumor which can be more difficult to remove.
Survival Rate
The surgical removal of the tumor is the main factor that can influence the person’s survival. Patients who have their tumors removed completely can approximately have a 5-year survival rate of about 67-80%. In patients with partial removal of tumors, they only have 22-47% survival rate in an estimation of 5 years.
References
- http://www.childhoodbraintumor.org/medical-information/brain-tumor-types-and-imaging/item/84-ependymomas
- http://www.abta.org/brain-tumor-information/types-of-tumors/ependymoma.html?referrer=https://www.google.com.ph/
- https://cern-foundation.org/?page_id=96
- Agbahiwe HC, Wharam M, Batra S, Cohen K, Terezakis SA (2013 Feb 1). Management of pediatric myxopapillary ependymoma: the role of adjuvant radiation. Int J Radiat Oncol Biol Phys85 (2):421-7.
- Amirian ES, Armstrong TS, Gilbert MR, Scheurer ME (2011 Sep 28). Predictors of survival among older adults with ependymoma. J Neurooncol.
- Merchant TE, Li C, Xiong X, Gaber MW (2008 Nov 17). Cytokine and Growth Factor Responses After Radiotherapy for Localized Ependymoma. Int J Radiat Oncol Biol Phys.
Similar Posts:
- Spinal Cancer – Symptoms, Prognosis, Survival Rate, Life Expectancy
- Medulloblastoma
- Inoperable Brain Tumor
- Homer Wright Rosettes
- Angiolipoma
- Anaplastic Astrocytoma
- Neuroendocrine Cancer – Symptoms, Treatment, Prognosis, Survival Rate






Leave a Reply